The Complications of Placenta Previa: Detailed Guide 2023
Placenta previa is defined as an unusually low-lying placenta that is in close proximity to or wholly or partly covering the internal cervical os. It is considered a crucial trigger in causing life-threatening antepartum and postpartum hemorrhage. Prompt identification and diagnosis can prevent hazardous outcomes and prove life-saving. Studies show an association with the spectrum of abnormal villous adherence (accrete, increta, and percent) in patients with placenta previa. The threat of uncontrolled hemorrhage can be a source of apprehension for the pregnant woman.
What are the Risk Factors Involved?
The consumption of contaminated placenta capsules can increase maternal GBS intestinal and skin colonization, which can be transferred to the infant. Therefore, it is recommended to avoid placenta capsule ingestion as the encapsulation process does not eliminate infectious pathogens.
Genevieve Howland shared on her blog Mama Natural that taking placenta pills resulted in a significant increase in her milk supply.
Alex Farr, who co-authored a review of human placentophagy, is from the Medical University of Vienna in Austria. It is known that most mammals consume the placenta after giving birth, but the reason for this behavior is uncertain.
Several risk factors have been associated with placenta previa, including:
- Previous placenta previa
- Prior induced abortion
- Prior spontaneous abortion
- Previous cesarean section
- Advanced maternal age
- Multiparity
- Maternal smoking
- Maternal use of cocaine
- Male fetus
- Assisted reproductive techniques (ART), including IVF and ICSI.
Pathophysiology in Complications of Placenta Previa
After placenta nutrition information previa results from the abnormal insertion of the placenta into the lower uterine segment in relation to the internal cervical os. The aforementioned risk factors play a role in compromising blood flow, thus resulting in abnormal implantation.
Not only does the placenta provide your baby with oxygen, but it also removes carbon dioxide and other waste products.
Generally, as the pregnancy progresses, the placenta migrates towards areas of high vascularity at the fundus, a process called placental trophotropism. This may be why 90% of “low-lying” placentas usually resolve as the gestational age advances. The distal placental portion at the lower uterine segment may eventually regress, atrophy, or persist as succenturiate lobe or vasa previa.
Classification
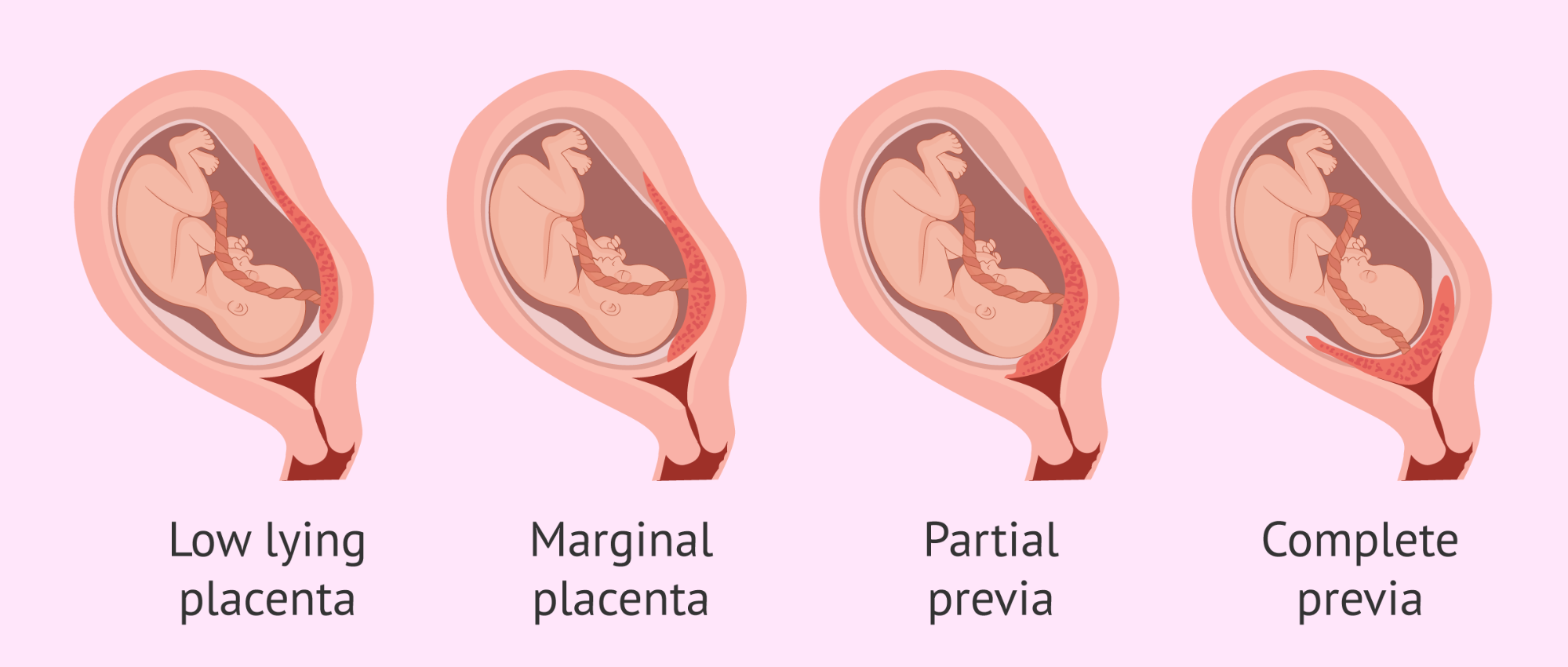
Placenta previa is classified into the following grades depending on its relation to the internal cervical os:
- Grade I – Low-lying placenta: placenta lies within the lower uterine segment, but its edge does not reach the internal cervical os (the border is within 2.0-3.5 cm from the internal os).
- Grade II – Marginal placenta: lower edge of the placenta reaches the internal cervical os without covering it.
- Grade III – Partial Previa: placenta partially covers the internal os.
- Grade IV – Complete Previa: placenta completely covers the internal os.
Symptoms, signs & evaluation
The most common presentation is painless bright red vaginal bleeding during the second or third trimester. Moreover, painless bleeding differentiates placenta previa from placental abruption, which presents with painful vaginal bleeding. Additionally, the bleeding may be elicited by sexual intercourse, gynecological examination, labor, or without apparent cause. However, not all patients with placenta previa experience this bleeding. Furthermore, accompanying uterine contractions may be present.
During per speculum examination, anywhere from minimal spotting to profuse bleeding may be revealed. It is important to avoid excessive examination with instruments or digital examination to prevent massive bleeding.
Transabdominal ultrasound scans during the first and second-trimester aid in the early detection and grading of placenta previa. Placental localization should be done at an 18-21 week anomaly scan.
However, follow-up scans between 28-32 weeks of gestation are recommended to establish the diagnosis due to placental trophotropism. Additionally, studies suggest transvaginal ultrasound is safe and more accurate in confirming the diagnosis. Sonography also aims at evaluating the presence of co-existing placenta accreta, increta, or percreta, thus helping decide appropriate management.
Furthermore, MRI remains the gold standard imaging modality for visualization of the placenta. Although costly, it has proven more convenient in posterior placenta previa cases and in detecting the placenta accreta spectrum.
Management
Placenta previa is a severe obstetric complication; moreover, vaginal delivery is ruled out. However, in cases of low-lying placenta, a trial of labor may be considered, albeit with an increased risk of postpartum hemorrhage. Therefore, thorough counseling of the patient regarding potential outcomes is crucial.
For established placenta previa, an elective cesarean section is scheduled at 36-37 weeks; however, complications may necessitate an earlier emergency cesarean section. Before delivery, arrangements should be made to handle massive hemorrhage, including blood matching and consent for uterine artery embolization/emergency hysterectomy if bleeding persists.
Additional interventions such as administering steroids for fetal lung maturity and magnesium sulfate for fetal neuroprotection may be advised by the attending obstetrician.
Complications of Placenta Previa
Placenta previa is associated with increased morbidity and mortality in both the mother and neonate.
Complications in fetus/neonate:
- Intrauterine growth restriction (IUGR)
- Preterm delivery
- Low birth weight
- Low APGAR score
- Respiratory distress syndrome
- Hypothermia
- Neonatal hyperbilirubinemia (jaundice)
- Major congenital anomaly
- Neonatal intensive care unit (NICU) admission
- Death
Complications in mother:
- Antepartum/intrapartum/postpartum hemorrhage
- The spectrum of abnormal placental villous adherence
- Premature rupture of membranes
- Surgical site infection after cesarean section
- Hysterectomy due to profuse hemorrhage
- Anemia secondary to hemorrhage
- Death
An insight from Mamahood
In conclusion, vaginal bleeding during any gestational age should not be taken lightly, and immediate consultation with your primary obstetrician should promptly diagnose placenta previa. Patients with established placenta previa should have multiple consultations with their obstetrician to discuss delivery, possible outcomes, and management plan to avoid future mishaps and mismanagement.