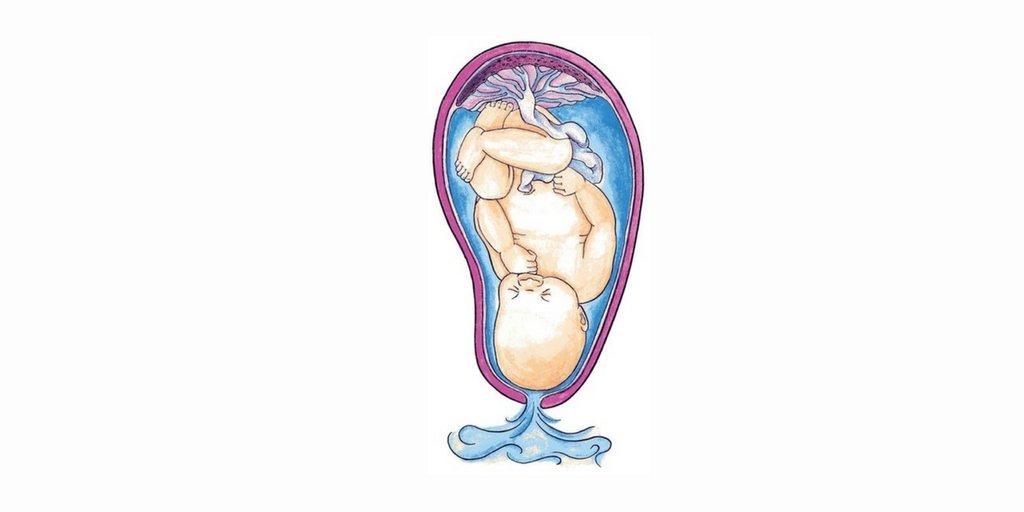
The breach in fetal membranes (amniotic sac and chorion) before the commencement of labor is referred to as premature rupture of membranes (PROM). If this rupture arises prior to 37 weeks of gestation, it is known as preterm PROM (PPROM). PROM is a pregnancy complication that affects approximately 8% of pregnancies at term. Similarly, 0.7-2% of pregnancies are complicated by preterm PROM.
What are the risk factors & etiology?
The exact etiology of PROM and PPROM is unestablished; however, several factors contribute to it. Uterine contractions leading to membrane weakening are a possible cause. Additionally, an association between intra-amniotic infection and PROM is observed.
Risk factors for PROM identified by studies include:
- Previous preterm delivery
- Short cervical length/need for cerclage (secondary to the incompetent cervix)
- Cigarette smoking
- Uterine overdistention (as with multiple gestations, polyhydramnios, etc.)
- Use of illicit drugs
- Low socioeconomic status
- Vitamin C and copper deficiency
- Second/third trimester vaginal bleeding
- Low BMI
- Connective tissue disorders
- Amniocentesis
- Multiparity
- Age <20 or >35 years
- Physiological abnormality of amniotic membrane
Pathophysiology
During labor, the fetal membranes undergo changes, including collagen breakdown and programmed cell death, ultimately weakening membranes, which, coupled with uterine contractions, causes the rupture of these membranes to facilitate fetal delivery.
In PROM, hastened membrane weakening is noted, likely brought about by increased collagenase and protease activity, the release of cytokines, an imbalance of metalloproteinases and tissue inhibitors of metalloproteinases, and, thus, a rise in intrauterine pressure.
History, physical examination & evaluation
The patient commonly presents with sudden painless leakage of vaginal fluid, which may be accompanied by pelvic pressure in the absence of contractions. Some may complain of vaginal bleeding also, which may be a manifestation of abruptio placentae.
Sterile measures while examining are to be ensured by obstetricians to minimize the risk of infection. Per speculum examination reveals the presence of fluid leakage from the cervical opening. Furthermore, speculum examination also detects umbilical cord or fetal prolapse, cervicitis signs, and the presence of vaginal bleeding.
Diagnosis of PROM/PPROM can be confirmed using a pH-detecting nitrazine test (amniotic fluid has pH 7.1-7.3) and crystallography on the leaked fluid. Ultrasound may demonstrate a low amniotic fluid index; however, the presence of normal liquor amount does not rule out PROM/PPROM. Additionally, ultrasound-guided intra-amniotic indigo carmine dye instillation is performed for diagnosis verification. If the injected dye stains a tampon/pad blue, it confirms that the fluid has passed through the vagina, thus establishing the presence of membrane rupture.
What are the complications involved?
PROM and PPROM jeopardize maternal and neonatal outcomes. Associated maternal complications documented are:
- Chorioamnionitis
- Endometritis
- Abruptio placentae
- Retained placenta
- Hemorrhage
- Increased risk of C-section
Preterm birth with PPROM is affiliated with the following:
- Perinatal mortality
- Fetal lung hypoplasia
- Respiratory distress syndrome
- Intraventricular hemorrhage
- Periventricular leukomalacia
- Retinopathy of prematurity
- Necrotizing enterocolitis
- Cerebral palsy
- Neurodevelopmental abnormalities
Management
Appropriate management is dictated by the gestational age of the patient. The following are the accepted guidelines:
- Term/Early term (≥37 weeks): Group B Streptococcus prophylaxis (as indicated) and delivery.
- Late preterm (34-36 weeks): Same as above.
- Preterm (24-33 weeks): Expectant management (observation), antibiotics, corticosteroids (single vs. rescue dosage depending on the institute), prophylaxis for GBS (as indicated)
- Pre-viability (<24 weeks): counseling of mother and family, expectant management/labor induction, antibiotics.
Tocolytic use is controversial, and although it may prolong the latency period and reduce the delivery risk for 48 hours, it is associated with an increased risk of infection (chorioamnionitis).
Magnesium sulfate lowers the risk of cerebral palsy and gross motor dysfunction.
Studies show that antibiotic use extends pregnancy and decreases maternal/fetal infections and fetal morbidity.
Corticosteroid use is shown to lessen neonatal mortality, respiratory distress syndrome, necrotizing enterocolitis, and intraventricular hemorrhage.
Mothers with a history of preterm delivery are recommended progesterone to prevent a recurrence.
An insight from mamahood
Mamas, PROM/PPROM is an unpredictable obstetric complication and can affect any expecting woman. Therefore, timely consultation is necessary as it ensures appropriate management, decreases infection risk, and reduces maternal and fetal morbidity.