In vitro fertilization (IVF), more popularly known as “test-tube” conception, is the commonest type of assisted reproductive technology (ART) used. The word in vitro in Latin translates to “within the glass” and refers to any technique that is performed outside of a living organism. IVF is the fertilization of oocytes in a petri dish. Originally designed to assist cases of untreatable fallopian tube disease, IVF is now widely used for infertility.
Indications
Infertility is the inability to conceive after 12 months of unprotected intercourse in women <35 years of age and after 6 months in women ≥35 years. It affects 10-15% of couples and can be due to male or female determinants. Factors resulting in failure to conceive and requiring IVF include:
- Tubal blockage
- Endometriosis
- Primary ovarian insufficiency (POI)
- Cervical factors –
- anti-sperm antibodies produced by females
- insufficient cervical mucus
- the thick consistency of cervical mucus
- Pelvic adhesions
- Male factors –
- low sperm count/abnormal morphology or motility
- sexual dysfunction
- hormonal imbalance
- congenital absence of vas deferens
- anti-sperm antibodies (autoantibodies produced by males)
- retrograde ejaculation
- testicular disorders (varicocele, spermatocele, tumors)
- Unexplained infertility
- Oocyte cryopreservation in women taking gonadotoxic medication (such as cancer treatment) who wish to preserve their fertility and those hoping to postpone childbearing.
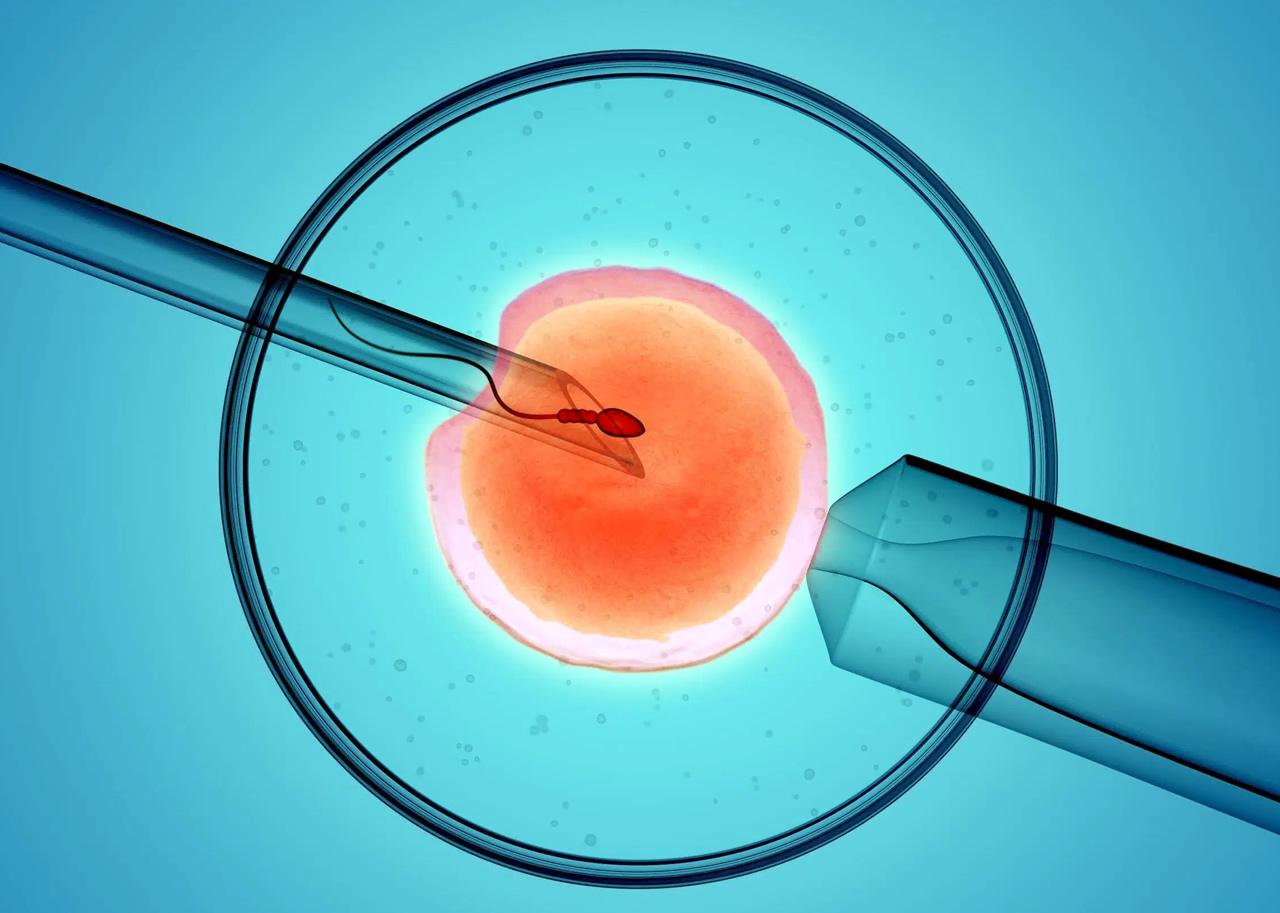
Intracytoplasmic sperm injection (ICSI) involves the injection of a single sperm into an oocyte using a micropipette. ICSI coupled with IVF may be indicated in the following:
- Azoospermia (absence of sperm from ejaculation)
- Oligospermia (low sperm count)
- Asthenospermia (Abnormal sperm motility)
- Teratospermia (Abnormal sperm morphology)
- Sperms recovered by TESA (testicular sperm aspiration)/TESE (testicular sperm extraction) techniques
- In the presence of anti-sperm antibodies
Contraindications
No absolute contraindications to IVF exist. However, any high-risk condition with an increased risk of morbidity and mortality in pregnancy (such as Eisenmenger syndrome, Marfan syndrome, Aortic coarctation, NYHA class 3 or 4 heart failure, pulmonary hypertension, severe valvular stenosis, etc.) should not undergo IVF. Women with these conditions who want biological children can opt for IVF with oocyte aspiration followed by fertilization with their partner’s sperm. Still, the embryo will be transferred to a surrogate.
Preparation
A thorough assessment and evaluation of the couple are necessary before IVF. Female oocyte ovarian reserve is estimated using cycle day 3 follicle-stimulating hormone (FSH) and estradiol (E2), anti-Mullerian hormone, or antral follicle count on cycle day 2-5 using ultrasound. If these tests reveal poor reserve, the woman can opt for IVF using donor oocytes.
Anatomic uterine abnormalities that may impact embryo implantation can be identified using imaging (Ultrasound/CT/MRI). Semen analysis is mandatory to decide on the use of ICSI. Both partners are recommended to undertake infectious disease screening (Hepatitis B/C, HIV, Syphilis).
Technique
Basic steps in IVF:
- Ovarian stimulation using clomiphene citrate, letrozole, or exogenous FSH and LH. Gonadotropin-releasing hormone (GnRH) analogs may be used to allow time for oocyte retrieval.
- Oocyte retrieval 33-35 hours after hCG injection via laparoscopy or transvesical ultrasound-directed oocyte recovery (TUDOR).
- Direct sperm collection or sperm retraction using TESA or TESE.
- Fertilization by incubating washed sperms and prepared oocytes for 12-18 hours or by ICSI.
- Embryo transfer is done on day 3 post-fertilization (cleavage stage) or on day 5 post-fertilization (blastocyst stage). Progesterone is prescribed for optimal implantation and pregnancy progression. Multiple embryos are transferred using a catheter into the uterus via the cervix under ultrasound guidance. Guidelines for the number of embryos to transfer as recommended by The American Society for Reproductive Medicine:
| Characteristics (age and prognosis) | Number of cleavage stage embryos to transfer | Number of blastocysts to transfer |
| <35, a most favorable outcome | 1-2 (1 recommended) | 1 |
| <35, the lesser likelihood of successful implantation | ≤2 | ≤2 |
| 35-37, the most favorable outcome | ≤2 | ≤2 |
| 35-37, the lesser probability of successful implantation | ≤3 | ≤2 |
| 38-40, the most favorable outcome | ≤3 | ≤2 |
| 38-40, the lesser likelihood of successful implantation | ≤4 | ≤3 |
| 41-42 years old | ≤5 | ≤3 |
Pre-implantation genetic diagnosis and genetic screening can be made to ensure the transfer of healthy embryos.
Complications
Studies show the following complications may arise with IVF:
- Ovarian hyperstimulation syndrome
- Multiple gestations – twins/triplets
- Pregnancy-induced hypertensive disorders
- Preterm delivery
- Gestational diabetes
- Antepartum hemorrhage
- Small for gestational age and low birth weight
- Increased risk of C-section
- Perinatal mortality
An insight from mamahood
We understand that IVF, although expensive, is a ray of light to all of you who wish to have children. Ladies, before proceeding with the decision of IVF, discuss all pros and cons with your healthcare provider to avoid treatment failure and to know the best available option in your individual case.